Staphylococcus bacteria manipulate the skin's natural protective mechanisms to provide themselves with optimal conditions for development, scientists from the Intercollegiate Faculty of Biotechnology of the University of Gdańsk and the Medical University of Gdańsk have determined.
The study on the mechanisms crucial for the proper functioning of the protective barriers of the human epidermis was carried out in collaboration with the University of Oxford, the Karolinska Institute and Imperial College London. The results were published in the Journal of Extracellular Vesicles.
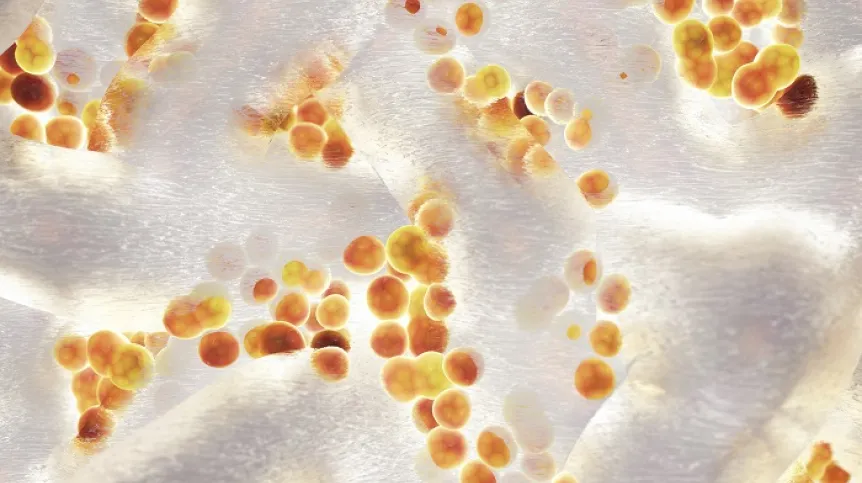
The skin is the largest organ of the human body - an adult human has about 2 square meters of it. 'The epidermis covering it, made of specialized cells (keratinocytes), can have up to several layers, the majority of its functions being performed by the upper layers of living cells and the upper stratum corneum, consisting of constantly exfoliating, dead keratinocytes. This layer of the epidermis prevents excessive evaporation of water and is responsible for maintaining proper acidity and limiting the growth of bacteria', the Foundation for Polish Science (FNP) says in a press release on its website.
Filaggrin plays a key role in the process of building the stratum corneum. This protein performs a number of functions in the skin, it is also responsible for mechanical strengthening of the epidermis. It programmatically kills the superficial cells, forming the stratum corneum.
'It is a kind of life-and-death switch for keratinocytes. However, this process must not happen too quickly. If it is activated too early, the barrier layer performing the necessary functions will not be formed. So the body has to control the levels of filaggrin when it is produced in the cells,’ says Dr. Danuta Gutowska-Owsiak from the University of Gdańsk and the first author of the study.
There is so much filaggrin in the upper layers of the epidermis that it forms granules that prevent intracellular release of the protein. Filaggrin is released from them into the cytoplasm only when the body is preparing to form the stratum corneum.
Until now, however, it was not clear how cells from the deeper layers of the epidermis protected themselves from premature death caused by excessive protein concentration, and only the latest work of the Gdańsk team showed that the deeper layers of the skin removed excess filaggrin using small extracellular vesicles (sEVs).
'They are like soap bubbles sent by cells. They were once believed to simply be used to remove toxic by-products of the cell's metabolism. Today, we know that they also have another function, they can transmit signals between cells and tissues of the body. After reaching the circulatory system, they can even go from the skin to the brain,’ says Dr. Gutowska-Owsiak.
Researchers have shown that Staphylococcus aureus, a common bacterium that exacerbates skin inflammation, is able to manipulate this process.
Filaggrin plays an important role in the prevention of atopic dermatitis (AD). The less of it in the skin, the higher the risk of this disease. This protein controls the multiplication ofstaphylococcus, because the products of its breakdown lower the pH of the skin, creating unfavourable conditions for the bacterium. In the case of a complete lack of filaggrin in the epidermis, the risk of AD is 150 times higher than with a normal concentration of this protein.
In the latest study, Dr. Gutowska-Owsiak's team shows that the presence of bacteria makes skin cells transfer filaggrin to sEVs faster. This causes the protein to be removed more intensively, resulting in its decreased concentration in the epidermis.
'We believe that in this way, the bacterium can eliminate this protein from the epidermis, which impairs the functioning of the skin barrier. Thus, staphylococcus manipulates the natural process to create living conditions for itself,’ Gutowska-Owsiak says.
In the future, these findings could lead to new treatments for AD, based on manipulating the mechanism that regulates filaggrin levels. They can also help in the development of new ways to prevent the development of allergies, which are also associated with pathological conditions of the epidermis.
Dr. Gutowska-Owsiak is one of the winners of the FNP First Team programme. The study was financed with funds from the First TEAM programme, as well as grants from the British Skin Foundation, Medical Research Council UK and the Polish National Science Centre.
PAP - Science in Poland
ekr/ bar/ kap/
tr. RL