Forces of nature can be used to treat organ fibrosis, say experts
 Photo from the Jagiellonian University press materials
Photo from the Jagiellonian University press materials
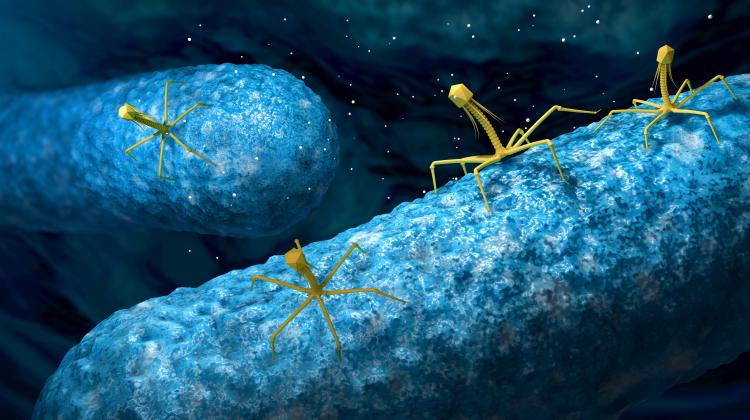
According to researchers from the Jagiellonian University, in the future it will be possible to treat organ fibrosis using the forces of nature. The researchers want to use extracellular vesicles, i.e. nanostructures secreted by cells of various organisms.
The team led by Dr. Sylwia Bobis-Wozowicz from the Faculty of Biochemistry, Biophysics and Biotechnology at the Jagiellonian University, discovered an important property of these structures and conducted research proving that the vesicles could potentially be used in therapy.
Extracellular vesicles are made of a lipid bilayer membrane that contains a rich mix of bioactive substances that have various effects on other cells of the body. The researchers from Kraków discovered that micro RNA biomolecules in extracellular vesicles have strong anti-fibrotic properties.
'We observed with in vitro and in vivo experiments that after the administration of extracellular vesicles there was a significant or complete reduction of proteins responsible for progressive tissue stiffening. In a model of cardiac fibrosis in experimental animals, we found that in some of the tested individuals, fibrosis in the heart completely reversed after just two weeks, despite the fact that during the same period they were stimulated with a factor causing fibrosis,’ says Dr. Bobis-Wozowicz.
The researchers believe that extracellular vesicles can be used to develop a new therapy for organ fibrosis. However, further preclinical research in this area is still necessary. 'Due to the high costs of such research, we are looking for entities from the pharmaceutical and biotechnology sector that would be interested in improving this technology and ultimately marketing it,’ says Dr. Gabriela Konopka-Cupiał, director of the Centre for Technology Transfer CITTRU at the Jagiellonian University.
The research focuses on micro RNA molecules responsible for the antifibrotic properties of extracellular vesicles. Dr. Bobis-Wozowicz's team has already identified them and confirmed that they act as an inhibitor of fibrotic processes.
'Micro RNAs affect mRNA molecules found in cells, which are the carriers of genetic information. mRNAs contain precise instructions for the production of specific proteins. The micro RNA biomolecules we have identified act in a specific way, inhibiting the production of those proteins that directly lead to fibrosis. Therefore, by administering the appropriate amount of a specific micro RNA to the areas of organs or cells overproducing fibrotic proteins, we can stop the development of the disease,’ says Dr. Bobis-Wozowicz.
The identified micro RNA works equally effectively in the treatment of fibrosis of various organs - heart, lungs, pancreas and liver. To apply this type of therapy, it is necessary to isolate extracellular vesicles. They can be obtained from cultures of the so-called induced pluripotent stem cells (iPSCs).
'IPSCs are obtained by reprogramming mature cells to a state of pluripotency using specific laboratory procedures. First, cells are collected from the patient, for example from fat tissue or blood. They are then reprogrammed into iPSCs, i.e. cells that can differentiate into various types of tissues,’ says Dr. Bobis-Wozowicz.
She explains that the obtained cells are cultured in special physiological conditions, and then vesicles are isolated from such cultures. The collected vesicles can be administered intravenously or placed in hyaluronic hydrogel, which is neutral to the body. This results in a preparation that can be injected into the affected area. The hydrogel form means that the vesicles will be released gradually over an appropriately extended period of time. 'This will ensure greater effectiveness of the therapy and a longer impact of extracellular vesicles on tissues prone to fibrosis,’ the expert says.
The team from the Jagiellonian University has shown that cultivating pluripotent cells in conditions of physiological hypoxia (with an appropriately reduced oxygen concentration) brings much better results. Vesicles obtained from such a culture have a much stronger therapeutic effect.
The medicinal preparation takes about two months. This is the case when the material for culture is taken from the same patient who is later injected with the obtained extracellular vesicles. 'The scientific literature clearly indicates that extracellular vesicles are not immunogenic, so it can be assumed that the medicinal material may come from cell cultures from different donors,’ say the Jagiellonian University researchers.
They emphasise that the donor does not have to be the same person who will ultimately take the drug. Therefore, there is a chance to implement the production of a universal drug on a larger scale and apply the therapy immediately after the doctor's recommendation. 'This would be possible because, as research has shown, vesicles tolerate storage very well, even over longer periods,’ the experts argue.
They also checked whether, for therapeutic purposes, it would be easier to synthesize appropriate micro RNA biomolecules and administer them in specially prepared lipid coats, instead of cultivating pluripotent stem cells.
'The calculations show that the variant of therapy with synthetic micro RNA, although technically it seems simpler, would cost several times more compared to the variant in which we grow stem cells and obtain natural extracellular vesicles from them. Moreover, the undeniable advantage of natural cultures is biocompatibility, and in the case of personalized therapies - complete elimination of the risk of unwanted immunological reactions to the administered preparation,’ says Dr. Bobis-Wozowicz.
The scientists add that the universality of the therapy should not be understood to mean that extracellular vesicles will be able to dissolve existing fibrosis or collagen deposits. Their function is strictly to inhibit fibrotic processes that occur, for example, in chronic inflammation of organs or during impaired production of fibrotic proteins.
They add that so far they have not detected any side effects of administering extracellular vesicles to the body. In vivo studies used, among others, mice with weakened immune systems. Importantly, no side effects were observed in their case either during drug administration or after completion of therapy.
Fibrosis is a progressive disease resulting from excessive production of extracellular matrix (ECM) proteins. These proteins, deposited in tissues, cause them to stiffen, which in turn leads to impaired functioning of organs. Fibrosis may occur, for example, in the heart, lungs, pancreas or liver.
It is estimated that fibrotic diseases are responsible for approximately 45% of all deaths in the world. So far, no effective cure for these diseases has been developed. Currently used treatment methods focus on eliminating the causes that induce chronic inflammation - e.g. the treatment of hypertriglyceridemia, treatment of chronic hepatitis B or C, the use of corticosteroids and drugs that suppress the immune system, and even removal of a fragment or entire organ affected by fibrosis.
Initially, it was thought that cells produced vesicles to remove unnecessary biomolecules or metabolites. Today we know that their role is much broader. Vesicles can penetrate other cells, which means that the biologically active ingredients they contain cause specific reactions. In this way, the contents of the vesicles are exchanged between cells, which consequently affects the biochemical cellular processes.
The signals transmitted in this way initiate various 'cell behaviours' - they intensify, support, inhibit or disrupt them - all depending on the instructions contained in the vesicles and the biochemical context in the target cells. Some of such signals have desirable effects, others - as in the case of 'messages' sent by cancer cells - are harmful and pathogenic.
Extracellular vesicles are studied in many centres around the world. They are a source of information about pathogenesis, cellular biochemical processes and properties of various types of cells. Analysis of the chemical composition of the contents of the vesicles may provide clues supporting the diagnosis of various diseases, the experts from the Jagiellonian University say. (PAP)
PAP - Science in Poland
zbw/ bar/ kap/
tr. RL
Przed dodaniem komentarza prosimy o zapoznanie z Regulaminem forum serwisu Nauka w Polsce.