Global warming and other environmental changes drive antibiotic resistance
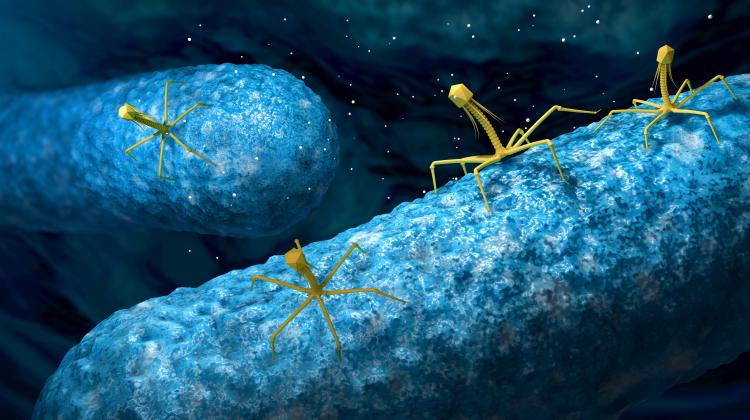
 Credit: Adobe Stock
Credit: Adobe Stock
Antibiotics are considered one of the greatest achievements of 20th century medicine. Their introduction reduced mortality due to bacterial infections and contributed to the extension of life expectancy. However, the consequence of their mass use in humans and animals is the emergence and spread of strains resistant to these drugs. According to estimates, in 2019, 4.95 million people around the world died due to antibiotic resistance, including nearly a million children.
In addition to the excessive and inappropriate use of antibiotics in animals and humans, environmental changes may contribute to the spread of resistance to these drugs. These include the warming climate, emissions of pesticides and heavy metals, microplastic pollution and changes in microbial diversity, Polish scientists report in the journal Environmetal Pollution (DOI: 10.1016/j.envpol.2024.123649).
'First of all, in conditions of rising temperatures, we can expect a higher incidence of bacterial infections and food poisonings, resulting in an increase in the consumption of antibiotics. Secondly, increased temperatures facilitate horizontal gene transfer, which involves the transfer of genetic information stored in plasmids. It may occur between bacteria of the same or different species. This is one of the most important ways of spreading antibiotic resistance genes. Thirdly, extreme weather phenomena resulting from a changing climate may damage sewage infrastructure, releasing untreated sewage. And these are an important source of antibiotics and resistant bacteria. As a result, the pool of resistance genes in the environment is enriched. And fourthly, a warming climate means a growing problem with access to safe drinking water, especially in regions with a lower level of economic development. It may result in an increased use of antibiotics, and expose people to drinking water contaminated with both antibiotics and resistant bacteria,’ says the first author of the paper, Professor Piotr Rzymski from the Department of Environmental Medicine, Poznan University of Medical Sciences.
The authors of the analyses point out that antibiotic resistance may also be driven by microplastic pollution. Hydrophobic surface of microplastics promotes the growth of bacteria, which is probably why horizontal gene transfer between bacteria occurs faster in their presence. Microplastics can also absorb antibiotics and transport them, along with resistant bacteria, over longer distances, especially in aquatic environments. 'The presence of resistance genes has been detected on the surface of microplastics found in both fresh and salt water ecosystems, leachate from landfills, as well as agricultural soil,’ says Professor Rzymski.
Exposure of bacteria to pesticides and heavy metals in the environment may, in turn, lead to the emergence and propagation of mechanisms that reduce the toxicity of these chemicals. 'It turns out that these mechanisms, based, for example, on enzymes involved in the degradation of organic pesticides or efflux pumps, make it possible to remove harmful compounds from the bacterial cell, but they may also play a role in reducing the sensitivity of bacteria to selected classes of antibiotics. This effect cannot be ignored, considering that every year human activity contributes to the emission of metals such as mercury, cadmium and lead, which can remain in the soil and water for a long time and accumulate in living organisms. In 2020 alone, the global consumption of pesticides in agriculture reached 2.7 million tons of active ingredients,’ says Rzymski.
Researchers also point to the important role of high microbial diversity in limiting the spread of antibiotic resistance in the environment. It creates a biotic barrier based on developed relationships between the organisms that form the community, the effective use of the pool of nutrients and the presence of organisms that can effectively control the development of antibiotic-resistant bacteria. If diversity is low, invasions of antibiotic-resistant bacteria and the spread of resistance genes among indigenous microorganisms may occur faster. The degradation of microbial diversity is facilitated by climate change, chemicalisation of the environment and its physical transformation.
'The objectives of public health and environmental protection converge, they must complement and enhance each other. Antibiotic resistance and environmental changes are among the greatest challenges for humanity in the 21st century and we should solve them together, not separately,’ says the publication’s co-author, Professor Andrzej Fal, president of the Polish Society of Public Health.
A growing challenge is bacteria resistant to more than one targeted antibiotic and to the so-called last-resort antibiotics. Particular threats include: multidrug-resistant tubercle bacilli, methicillin-resistant strains of Staphylococcus aureus, vancomycin-resistant enterococci and Clostridioides difficile, carbapenem-resistant enterobacteria and colistin-resistant Gram-negative bacteria. (PAP)
PAP - Science in Poland
zan/ agt/ kap/
tr. RL
Przed dodaniem komentarza prosimy o zapoznanie z Regulaminem forum serwisu Nauka w Polsce.