Strengthen the heart after heart attack: the Polish method for stem cells
 Photo: Fotolia
Photo: Fotolia
It is possible to strengthen the heart after a heart attack with stem cells. Scientists from Poznań have shown how to genetically modify stem cells to better support the work of the heart. Now they are investigating the effectiveness of this procedure in detail.
The heart is a muscle that should work throughout life without interruption. Its cells must be well supplied with nutrients. If there is an embolism in any of the coronary arteries that surround the heart and supply it, the cells which the blood does not reach will die. Such heart cell necrosis is called a heart attack. About 15 thousand people die every year in Poland due to a heart attack. If the patient survives, a scar forms in the heart. It is not built of muscle tissue, but of connective tissue. These cells are less flexible and do not help the heart function. The wall of the heart is thinner in this place, and more susceptible to tearing.
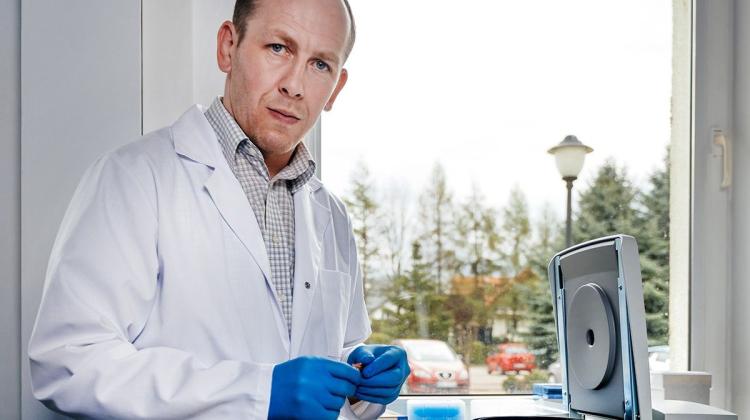
Professor Maciej Kurpisz from the Institute of Human Genetics PAS in Poznań says that stem cells can be delivered there to strengthen heart function after a heart attack - especially in people who are not eligible for surgery. These cells can reproduce freely, and their role in the body is not defined yet. Thus, they can transform into cells of various types.
Stem cells are collected from the patient`s thigh muscle. They are multiplied, and then delivered with a catheter to the damaged areas in the heart. Until now, however, such treatments have not been very effective. Stem cells would not bind well to myocardial cells.
TELL STEM CELLS WHAT TO DO
Meanwhile, Polish scientists have shown what genetic modifications should be performed on stem cells to make them support the heart more effectively. Their paper was published in 2017 in the European Journal of Heart Failure.
"Cells are modified so that they form the tissue characteristic of the heart - cardiac sarcomeres" - says Prof. Kurpisz.
He adds that the modification concerns the gene from human muscle cells.
"We`re conducting a therapeutic medical experiment on people who are not eligible for heart transplant" - the professor says. The idea is patent-pending. Professor Kurpisz mentions that in the future this solution could be used by people after a heart attack, who are not eligible for transplant or by-pass, people with low ejection fraction (less than 30%) and people struggling with disease following a heart attack.
HEART AS GOOD AS NEW
The geneticist describes the procedure. Once the stem cells are collected from the patient, modified and multiplied, the heart is mapped. "The examination is similar to coronography" - compares the geneticist. Once the doctors know where the heart is weak - less contractile - stem cells are delivered to that spot with a special needle. "Patients say that they feel a small sting. After two days the patient can go home, just like after coronography" - says Prof. Kurpisz.
Stem cells are delivered to those areas in the heart where there are no other muscle cells. New muscle cells have conditions to multiply. "When they reach the muscle cells of the heart, they bind to them with cytoplasmic bridges - thanks to our genetic modification" - describes the geneticist.
QUALITATIVE LEEP THANKS TO THE BRIDGES?
"It is a qualitative leap. Until now stem cells would not attach to myocardium cells as we would like them to, and because of that they did not produce a good electrical potential" - says Prof. Kurpisz.
The problem is synchronization with other heart cells. "This, in turn, caused additional arrhythmia" - adds the geneticist. In his opinion, cytoplasmic bridges resulting from genetic modification synchronize the work of old and new cells.
"Our patients do not have arrhythmia, their cells bind to the heart cells" - says the geneticist.
Researchers from his team want to confirm the effectiveness of their solution in further, more detailed studies.
TRACKING STEM CELLS WITH SPIONS
Scientists from Poznań want to see how the stem cells delivered during the procedure actually move in the body. To determine that, they want to use superparamagnetic iron oxide nanoparticles (SPIONs). Publication on this topic appeared in "Scientific Reports". Both in vitro and in vivo tests are planned.
Professor Kurpisz explains that nanoparticles that penetrate into cells (including stem cells) are easy to track in the body, for example using magnetic resonance. Tracking them will tell how many of the cells delivered during the procedure actually attach to the heart, and how many do not. Researchers plan to test nanoparticles in a pre-clinical model - in a pig`s body. If the tests are successful, they can start the first tests on humans.
Professor Kurpisz hopes that in the future SPIONs can be used for controlled point delivery and release of drugs.
PAP - Science in Poland, Ludwika Tomala
lt/ agt/ kap/
tr. RL
Przed dodaniem komentarza prosimy o zapoznanie z Regulaminem forum serwisu Nauka w Polsce.