Polish researchers developed a method of producing hybrid organs
 Photo: Fotolia
Photo: Fotolia
Researchers from Lodz University of Technology have developed an original method of producing so-called hybrid organs that can potentially replace or support, for example, damaged pancreas, liver, thyroid or parathyroid glands.
Polymer macrocapsules with living cells that they have produced can be used, among other things, to assist patients waiting for organ transplants.
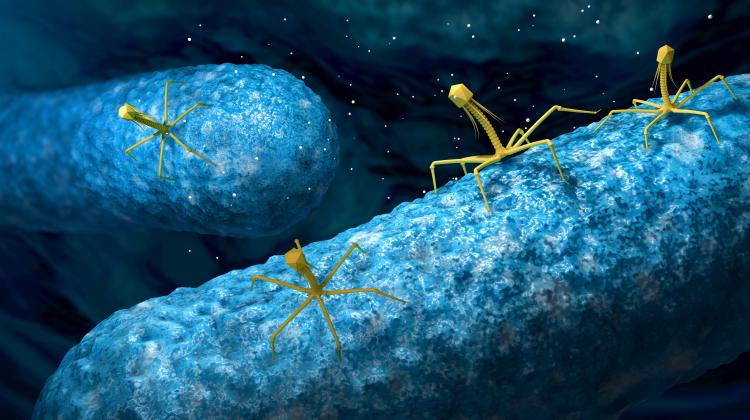
The researchers patented a method of making capsules with living cells derived from the same species (allogeneic), or from a different species (xenogeneic), the structure of which protects them from the effects of some factors of the immune system of the recipient that are responsible for graft rejection. This design allows for the nutrition of all encapsulated cells, preventing their death, and allows the products of cell metabolism to be transferred outside the capsule.
"This solution is original on a global scale, relatively simple, and yet very interesting in its design" - told PAP co-author of this method, Prof. Marek Kozicki from the Department of Man-Made Fibres, Lodz University of Technology.
The deficit of organs for transplantation, graft rejection and complications arising from taking immunosuppressants after transplantation are the causes of the search for alternative methods of supporting patients. Hybrid organs, or transplantation of encapsulated cells, is considered a promising method for replacing or supporting organs such as endocrine glands, including pancreas, liver or parathyroid glands.
"A hybrid organ is a polymer system with enclosed living cells, intended to assist damaged organs such endocrine glands: pancreas, liver, thyroid or parathyroid glands. The essence of this structure is to protect the allogeneic or xenogeneic cells from the main factors of the immune system of the recipient" - explained Prof. Kozicki.
The original structure of the hybrid organ has been developed at Lodz University of Technology by the team led by Prof. Janusz M. Rosiak. The essence of this organ is a three-layer polymer capsule.
"We have the inner multi-cellular core with a very complex structure, which consists of hundreds of microscopic bubbles, in which live cells can easily replicate. The core of the macrocapsule is surrounded by polymer membranes that strengthen it and protect encapsulated cells. At the same time, they ensure free diffusion of nutrients to the cells and diffusion of the substances produced by encapsulated cell into the patient\'s body" - described Prof. Kozicki.
Both the core and the shells are made from natural, biodegradable polymers. An additional third layer may be the outer sheath of synthetic, non-biodegradable polymer. Autologous (from the same person) and isogenic (from genetically identical person, e.g. twin) cells can be implanted in biodegradable shells, and the third, synthetic polymer shell allows to use also allogeneic and xenogeneic cells.
How do researchers obtain such macrocapsules? Cells isolated from the target organ, for example pancreas or liver, are mixed with the polymer solution with appropriate chemical composition that prevents the cells from being destroyed. Then the polymer solution with cells is dripped into the forming solution.
"As a result of the reaction, contact of the polymer containing the cells with the forming solution, capsules containing living cells form automatically" - the researcher explained. The next step may be applying additional protection in the form of polymer membranes - natural and synthetic.
The structure of macrocapsules developed at Lodz University of Technology is - according to the authors - unique and has at least one advantage over other available solutions: multi-chamber internal structure, consisting of hundreds of microscopic bubbles, voids, in which the cells can multiply, allowing all cells to be nourished.
"If cells multiply in the middle of the capsule, nutrients can reach the cells" - emphasised Prof. Kozicki. Thus, the structure of the Polish macrocapsule improves the survival rate of the transplanted cells and allows to avoid the problems associated with rapid dying of malnourished cells.
The capsules were tested in in vitro tests of cell proliferation and cellular structures, i.e., Saccharomyces cerevisiae (yeast), fibroblasts, follicular thyroid, islets of Langerhans (pancreas). They were also tested in vivo, for tolerance in organisms of Wistar rats.
"The results were very good, we observed the formation of networks of blood vessels around these structures - implanted capsules, and no rejections" - said the scientist. Rats were implanted, among others, with macrocapsules containing xenogeneic thyroid bubbles after complete resection of the thyroid gland, and after 2 weeks normalization of thyroid hormone levels in the peripheral blood of animals was observed.
According to another co-author of the solution, Dr. Marek Kołodziejczyk, MD, the multi-cell hybrid organ system allows to implant the cells previously propagated in vitro and encapsulated, which, by secreting appropriate substances after implantation, can save patients waiting for an organ transplant.
Coatings that provide immunoprotection prevent the cells inside the capsule from being destroyed, allowing to use not only autologous cells obtained (if possible) from the patient and not requiring immunosuppressive drugs, but also allogeneic cells (obtained from unrelated donor) or xenogeneic (animal) cells, without the need for immunosuppressants after implantation of such protected cells into the recipient\'s organism - added Dr. Kołodziejczyk.
Scientists from Łódź argue that they have not seen a similar solution in the world literature. They would like to raise funds for further development, further research and building a device for the production of hybrid organs.
"It is necessary to work with other partners in Poland. Our team encourages other professionals to read this study, which is really attractive compared to other studies in the world" - said Prof. Kozicki.
PAP - Science and Scholarship in Poland, Kamil Szubański
szu/ pmw/ laz/ hgt/ mrt/
tr. RL
Przed dodaniem komentarza prosimy o zapoznanie z Regulaminem forum serwisu Nauka w Polsce.