Human testing of prostate cancer vaccine developed by Polish scientist

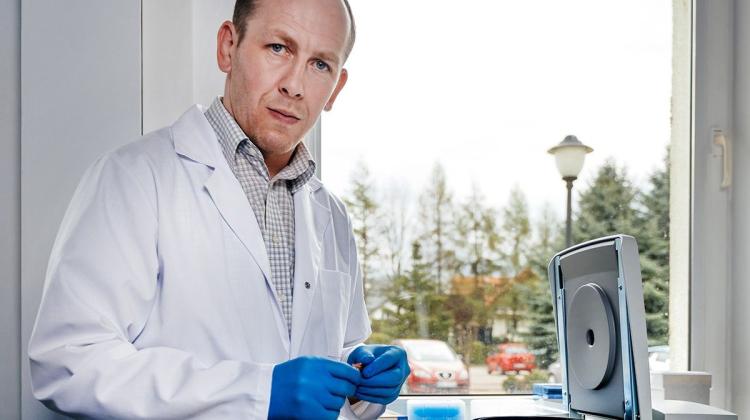
Therapeutic vaccine for prostate cancer, which was developed by a team of scientists from Germany led by Polish scientist, is undergoing clinical trials in humans. The study takes place in eight EU countries, including Poland.
"In Poland, we want to include as many patients as possible in the study. We are planning to finish recruitment by the end of 2013" - told PAP Dr. Mariola Fotin-Mleczek, chief scientist at CureVac, the company that developed the vaccine. She noted that because of the more complex bureaucratic procedures, Poland was the last country to join the study. Currently, tests are carried out in Germany, Sweden, Switzerland, United Kingdom, France, Spain and the Czech Republic.
A CHANCE FOR PATIENTS
The expert explained that patients invited to test the new vaccine are men with advanced prostate cancer, in whom standard hormonal therapy is no longer effective (the so-called prostate cancer resistant to castration) and progression of the disease has occurred, but who are not yet eligible for chemotherapy. "At present in Poland there are virtually no treatment options for these patients. The only thing they are offered is waiting and observation. Only when the progression of the disease is high, they receive chemotherapy, which is associated with extensive indeed adverse effects" - said Dr. Fotin-Mleczek.
In an interview with PAP, Iwona Skoneczna, head of the Polish office of the European Organization for Research and Treatment of Cancer (EORTC) at the Institute of Oncology in Warsaw reminded that clinical trials are often presented in a negative light by the media. "However, they should be rather perceived as a chance for patients. They often offer great benefits for patients, who gain access to the most promising new treatments. In some cases, for months patients receive innovative medicines, which will not quickly appear on reimbursement lists, and they are covered by a very good medical care" - she said.
She noted that these patients often for many months, sometimes even years, do not need to use the resources of the National Health Fund, since during the clinical trial the costs of treatment and tests are covered by the manufacturer of the new drug, which also means additional financial benefits for hospitals.
Dr. Skoneczna pointed out that at present none of the four new drugs for advanced prostate cancer registered by the European Medicines Agency (EMA) after 2010 (cabazitaxel, abiraterone acetate, enzalutamid and alpha radin) is currently available for Polish patients, due to the lack of a refund. The only opportunity to take advantage of these drugs is to participate in clinical trials. As a result, hundreds of Polish patients could receive or continue to receive these drugs.
According to Dr. Fotin-Mleczek, earlier stages of testing the new vaccine have shown that it is well tolerated and does not cause serious adverse events. At most, local reactions like with other vaccines are observed, such as skin reaction or increased temperature. Importantly, it induces a strong immune response - after vaccination, the body produces immune cells capable of recognizing cancer cells and destroying them.
"As physicians who meet patients in need of new therapies every day, we are always glad when Polish patients have an opportunity to take advantage of any additional chance. Immunotherapy is useful in patients with advanced prostate cancer, and the new vaccine entering the study seems promising and much easier to use than the registered sipuleucel-T (the first therapeutic anti-cancer vaccine - PAP), although we will have to wait for the final results of the study" - believes Dr. Skoneczna, who participates in the research project.
More about the study can be found at the U.S. National Institutes of Health website that contains a database of information on ongoing clinical trials (http://clinicaltrials.gov/show/NCT01817738).
MIMIC A VIRUS
The researcher explained that the vaccine she developed is the first to use mRNA (messenger ribonucleic acid), that is a matrix copied from DNA that contains information about the protein that should formed in the cell. Research conducted and published 13 years ago by Dr. Ingmar Hoerr, the company\'s founder, have shown that mRNA introduced into the body from the outside is capable of inducing an immune response against the protein that is written in it.
Tested vaccine contains mRNA for six proteins, so-called antigens, that are specific to prostate cancer cells.
"This distinguishes it from other similar formulations , which are based on a single antigen, such as PSA or PAP. In this product, we have both these antigens, plus four others" - explained Dr. Fotin-Mleczek.
She noted that this is the more important that it give patients a better chance of getting multilateral immune response against tumour cells. "We must remember that not all of these antigens are present on the patient’s cancer cells. And secondly, cancer cells use escape mechanism - they reduce the production of antigens and thus become invisible to the immune system. Therefore, if we have six different antigens in the vaccine, there is a greater chance for effective immune system attack on cancer cells" - said the researcher.
She said that normally our immune system handles well the identification, capture and elimination of mutated cells that can initiate cancer development. If it didn’t, the occurrence of cancer would be much higher, because these dangerous cells form in our body every day in large quantities.
"Only in certain cases the immune system fails and begins to tolerate mutant cells, which leads to tumour progression" - said Dr. Fotin-Mleczek.
The task of the new vaccine, like other immunotherapy, is to mobilize the immune system to recognize and fight them.
Use mRNA for this purpose is reasonable as mRNA stimulates the immune response very well by mimicking a viral infection. "mRNA from outside the body constitutes a very dangerous signal for the immune system because it typically comes from viruses that have genetic material also in the form of RNA. Therefore, the immune system cannot afford to tolerate this signal" - explained the expert.
This means that the vaccine can be administered multiple times and each time the immune response increase is observed - i.e. the increase in the number of immune cells ready to combat cancer. "Every time you we vaccinate, we put the immune system on maximum alert. We teach it that the antigen, which has so far been tolerated in the body, is dangerous and cells that have it have to be eliminated" - said Dr. Fotin-Mleczek.
CELL MEMORY
According to Dr. Fotin-Mleczek, early doses are administered intradermally quite frequently - once a week, and then the intervals between them are increased.
"The important thing is that we do not end vaccination, even if the patients start using chemotherapy because of progression. It is not a contraindication. Only if after adding chemotherapy the disease continues to develop, we discontinue vaccinations" - explained the researcher.
In her opinion, this does not mean that the patient stops to benefit from vaccination. "Under the influence of vaccine, immunological memory calls were produced that can still be effective" - noted Dr. Fotin-Mleczek. This is the same type of cells that makes many vaccines given in childhood provide us with protection against infectious diseases for a lifetime.
Memory cells are important in fighting cancer because they are better adjusted to killing cancer cells. They are also more resistant to chemotherapy and irradiation. The new vaccine may therefore be combined with chemotherapy, because it does not destroy the entire pool of memory cells. Moreover, these cells - if necessary - divide and recreate much faster than other immune cells.
The test vaccine does not use any auxiliary material for the introduction of mRNA, which in itself could trigger an immune response, and "divert attention" from the core antigen. This ensures that after the vaccine is administered, the immune response is targeted only as desired. However, in addition to the mRNA of six different antigens, it also comprises the same mRNA molecules in complex with a protein, which act as an adjuvant, amplifying the response after vaccination.
This allows the vaccine to activate two types of immune response: congenital, which is more primal, quite fast and less specific (connected with a general activation of numerous immune cells such as monocytes, macrophages, granulocytes, NK (natural killer) cells) and acquired response, specific, i.e. associated with the production of lymphocytes T and B (which produce specific antibodies), responsible for immunological memory. For each antigen, different immune cells that recognize it are formed.
Only currently registered (U.S. only) cancer vaccine (for advanced prostate cancer) called sipuleucel-T (PROVENGE) uses modified dendritic cells. They are extracted from the patient\'s blood and transformed ex vivo in order to present a single PAP antigen, therefore this procedure is much more complicated, and the vaccine itself very expensive, because it must be prepared individually for each patient.
MRNA-based vaccines do not need to be produced individually the for each patient.
"Currently we are conducting research on a similar vaccine for lung cancer. We are using the same production line, you only need to change the sequence of the gene, which is used as a template" - explained the expert.
In her opinion, in the future this type of immune therapy can play a very important role in the various stages of cancer. At an early stage, before metastases occur, vaccine could be used after excision of the tumour to teach the immune system to combat single tumour cells that circulate in the body and try to infect it. This would prevent the formation of metastases. At a later stage of the disease, immune therapy may be combined with conventional therapies, such as chemotherapy and radiotherapy. This way, using various mechanisms and supporting each other, these therapies would more effectively eliminate cancer cells.
PAP - Science and Scholarship in Poland, Joanna Morga
jjj/ tot/ mrt/
tr. RL
Przed dodaniem komentarza prosimy o zapoznanie z Regulaminem forum serwisu Nauka w Polsce.